factors
The Biopsychosocial Approach to EDs
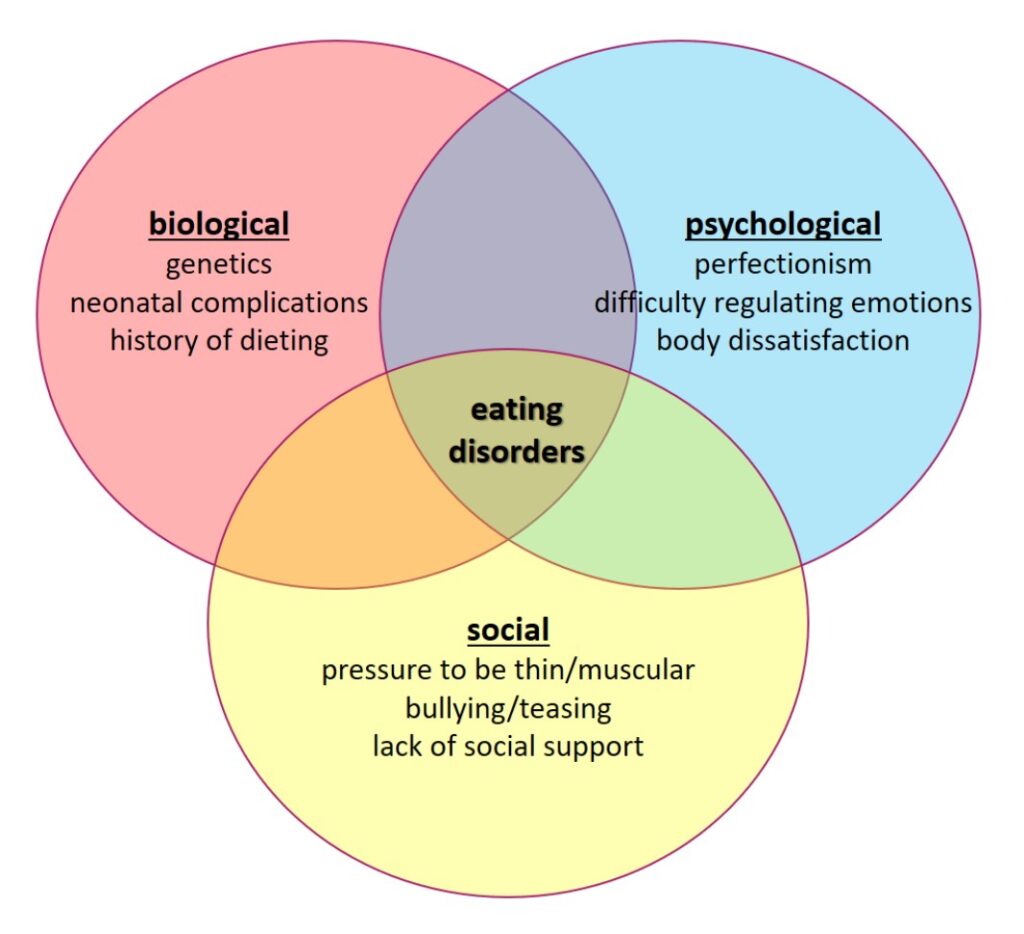
The biopsychosocial approach illustrates a combination of biological, psychological, and social factors that contribute to a more holistic understanding of disease and disorder pathology. It helps eating disorder clinicians and experts outline the connections between genes and environment to develop advanced treatment methods. Like many things, the complex interaction of eating disorder factors in an individual isn’t perfectly understood. For a longer list of factors in each of the three categories, check out withinhealth’s What Causes An Eating Disorder: A Biopsychosocial Perspective.
The Biological Side
Eating disorders have a significant biological component that isn't as well known by the general public. A family history of EDs can increase the likelihood that the environment will trigger the eating disorder in the child or teen. Abnormal brain activity and structure are also at work in people with EDs.
Family History of EDs
Eating disorders are mental health disorders, meaning genetics contribute considerably to the risk of ED development. In fact, genetics account for about 60% of ED risk. People with a mom or sister who have anorexia are up to 12 times more likely to develop it later on. Studies have also found that identical twins are more likely to develop an ED, compared to non-twin siblings or fraternal twins.
Brain Activity & Structure
Brain structure and activity play essential roles in ED development. The hypothalamus in particular, which helps control hunger signals, may not result in normal feelings of satiation in bulimics. Neurotransmitters, chemicals that attach to receptors in the brain to control mood, eating, etc., affect ED sufferers on a biological level. Serotonin, a neurotransmitter that helps regulate mood and appetite, has been found to be lower in people with EDs that involve binging episodes.
The Psychological Side
A significant part of eating disorder development has to do with the workings of people's thoughts. Anxiety, low self-esteem, and poor body image can set the stage for dangerous dieting behaviors which, in combination with inherited traits, may become an eating disorder.
Anxiety
Anxiety has high comorbidity with eating disorders, especially in anorexia nervosa (AN). In other words, people who already deal with an anxiety disorder are more likely to develop an eating disorder. Obsessive compulsive disorder (OCD) and generalized anxiety disorder are two such disorders that have a relationship with eating disorder development after childhood. Sensitive comments and observations from the environment related to eating and weight may be negatively-perceived and internalized by perfectionistic or anxious individuals.
Body Image
Body image describes how you associate with the size, shape, etc. of your body, whether it be positively or negatively. Poor body image is both a precipitating AND perpetuating factor of eating disorders: it both increases the risk of disorder development AND aids in its continuation. Body dysmorphia occurs when people distort the appearance of their body, blowing small flaws out of proportion, and is related to poor body image.
The Social Side
In anorexia, positive social feedback like compliments on weight loss can further encourage dangerous food restriction and eating habits, while in bulimia and binge-eating disorder, negative social feedback like rude comments on weight gain may foster shame... and shame drives binge-eating episodes. While family and peer relationships can negatively impact a person’s perception of their body and weight, it's important to note that families are not to blame, and can be the patients’ and providers’ best allies in treatment. Media influences, especially as seen in Southeast Asia, may facilitate social stress surrounding the “reward” of achieving the ideal body standard portrayed by famous figures. Exposure to food restriction (e.g., religious fasting) and excessive food intake (e.g., holiday meals, family traditions) resulting in rapid or dramatic weight change may bring feelings of dissatisfaction about body appearance to the surface.